Introduction: Several new therapeutic agents have been approved in recent years for the treatment of relapsed/refractory (R/R) Large B cell lymphoma (LBCL) (diffuse large B cell lymphoma [DLBCL] and high-grade B cell lymphomas [HGBCL]), such as new monoclonal antibodies (MA), bispecific antibodies (BA) and CAR-T cell therapy. The objective of our study was to evaluate the epidemiology and the use of these new therapies (NT) in Spain and to analyze the impact on survival.
Methods: We present a multicenter retrospective study based on the GELTAMO (Spanish lymphoma group) RELINF platform. From 60 centers actively registering on the platform, 17 university hospitals accepted to participate, and 5 of them were CAR-T therapy providers. Participating centers completed a short questionnaire on disease relapse and the use of new drugs in their registered patients. The histologies included were DLBCL, HGBCL not otherwise specified (NOS), and double hit (DH).
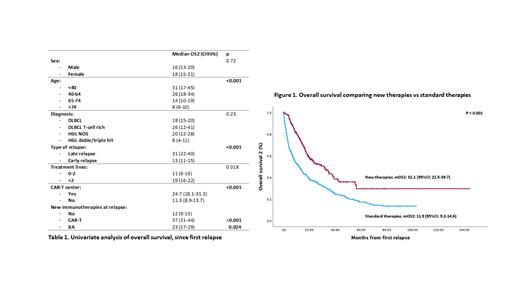
Results: From 3270 patients with ABCL registered, 2853 patients were included in the present analysis; 738 patients experienced R/R disease, 492 (67%) were refractory or had early relapse (up to 1 year from the first line), and 246 (33%) late relapses, half of them (54%) during the second year. In both early and late relapse groups, about a third of patients were older than 80 years. Early relapses were significantly higher in double/triple hit HGL (34%) and T-cell-rich DLBCL (29%) compared to DLBCL or HGL NOS (16%) (p<0.001). The median number of lines among relapsed patients was 2 (1-10). 236 patients received NT, with the following distribution: CAR-T, n=144, BA, n=68, polatuzumab-based, n=92, and tafasitamab-lenalidomide, n=14. Most patients who received only 2 lines (n=376) were treated with conventional treatments, although 11 patients (3%) received CAR-T, 11 (3%) BM, 15 (4%) polatuzumab-based, and 5 (1%) tafasitamab-lenalidomide. Among 354 patients who received more than 2 lines of treatment, 130 (37%) received CAR-T cell therapy, 75 (21%) polatuzumab, 9 (2%) tafasitamab-lenalidomide, 55 (15%) BA, and 160 (45%) of these patients did not receive any NT. In the overall series, with a median follow-up of 49 months (95%CI: 47-51), median progression-free survival (PFS) was 54 months (95%CI: 48-61), and median overall survival (OS) was 82 months (95%CI: 74-90). Considering only the R/R patients, with a median follow-up of 40 months since the first relapse, the median OS2 (mOS2) was 16.8 (IC95%: 14.5-19) months. Survival analysis is shown in Table 1. The mOS2 for the early relapse group was 13.5 (95%CI: 11.5-15.5) months vs 31.1 (95%CI: 22.5-39.8) months for late relapses. Median OS2 for relapsed patients treated with NT was 31.1 months (95%CI: 22.5-39.7) compared with 11.9 months (95%CI: 9.2-14.6) for the group of standard treatment (p<0.001)) (Figure 1). Interestingly, OS2 was longer in patients treated in CAR-T provider centers than in non-CAR-T centers, in both early relapse group (mOS: 18.3 months [95%CI: 14.1-22.5] vs. 8.6 months [95%CI: 6.2-11]: p<0.001) and late relapse group (37.9 months [95%CI: 24.2-51.5] vs. 18.7 months [95%CI: 13.9-23.4], p=0.001). This difference was not found when we evaluated high complexity institutions (those that perform allogeneic transplant) vs. those that are no. In multivariate analysis, early relapse (HR 1.68, 95%CI 1.37-2.06, p<0.001), age over 65 years (HR 1.91, 95%CI: 1.23-2.98, p=0.004), treatment with CAR-T cell therapy (HR 0.68, 95%CI: 0.51-0.90, p=0.007) and treatment in a CAR-T cell provider center (HR 0.7, 95%CI: 0.58-0.85, p<0.001) independently influenced OS2.
Conclusions: Our real-world analysis confirms the negative impact on OS of factors like age or early relapse in patients with R/R LBCL. According to our results, the introduction in recent years of NT has markedly improved OS, especially CAR-T cell therapy.
Disclosures
Bastos-Oreiro:BMS, Kite, Novartis, F. Hoffmann-La Roche Ltd, Incyte, Abbvie: Honoraria, Speakers Bureau; F. Hoffmann-La Roche Ltd, Kite, SEHH, AMHH: Research Funding; Incyte, Kite: Consultancy; Gregorio Maranon Hospital: Current Employment, Membership on an entity's Board of Directors or advisory committees; SEHH, AMHH: Membership on an entity's Board of Directors or advisory committees. Cordoba:European Hematology Association (EHA), Spanish Society Hematology (SEHH): Membership on an entity's Board of Directors or advisory committees; F. Hoffmann-La Roche Ltd, Takeda, Abbvie, Janssen, AstraZeneca, Lilly, BeiGene, BMS, Genmab, Incyte, Gilead: Speakers Bureau; F. Hoffmann-La Roche Ltd, Takeda, Abbvie, Janssen, AstraZeneca, Lilly, BeiGene, BMS, Genmab, Incyte, Gilead: Consultancy; Fundacion Jimenez Diaz University Hospital: Current Employment. Lopez Garcia:Beigene: Consultancy; Roche: Consultancy, Speakers Bureau; Janssen: Consultancy, Speakers Bureau; Astrazeneca: Consultancy, Speakers Bureau. Lopez-Guillermo:F. Hoffmann-La Roche Ltd, Gilead/Kite, Genmab, Celgene, Abbvie: Consultancy; Gilead/Kite, F. Hoffmann-La Roche Ltd: Research Funding; F. Hoffmann-La Roche Ltd, Gilead/Kite: Honoraria; GELTAMO (Spanish group of lymphomas, chair), Spanish Society of Hematology (vice-chair): Membership on an entity's Board of Directors or advisory committees. Martín García-Sancho:Roche: Consultancy, Honoraria; BMS/Celgene: Consultancy, Honoraria; Kyowa Kirin: Consultancy; Novartis: Consultancy; Gilead / Kite: Consultancy, Honoraria; Incyte: Consultancy; Janssen: Honoraria; Lilly: Consultancy; Miltenyi: Consultancy; ADC Therapeutics America: Consultancy; Ideogen: Consultancy; Abbvie: Consultancy; Sobi: Consultancy, Honoraria; Takeda: Honoraria; Eusa Pharma: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal